Why a Preventative Approach to Heart Health Matters More Than Ever

Heart disease remains the leading cause of death worldwide. But what’s often overlooked is that many of the risks tied to cardiovascular problems are not inevitable. They are manageable—and in many cases, preventable. While treatment after a heart-related event is critical, prevention is where we have the greatest power. The sooner we take our heart health seriously, the better our chances of avoiding complications later in life.
A preventative approach to heart health doesn’t just mean avoiding greasy food or jogging once in a while. It’s a full-spectrum strategy involving stress management, cholesterol and lipid control, and inflammation reduction. Let’s break this down into actionable, understandable areas so you can start protecting your heart today.
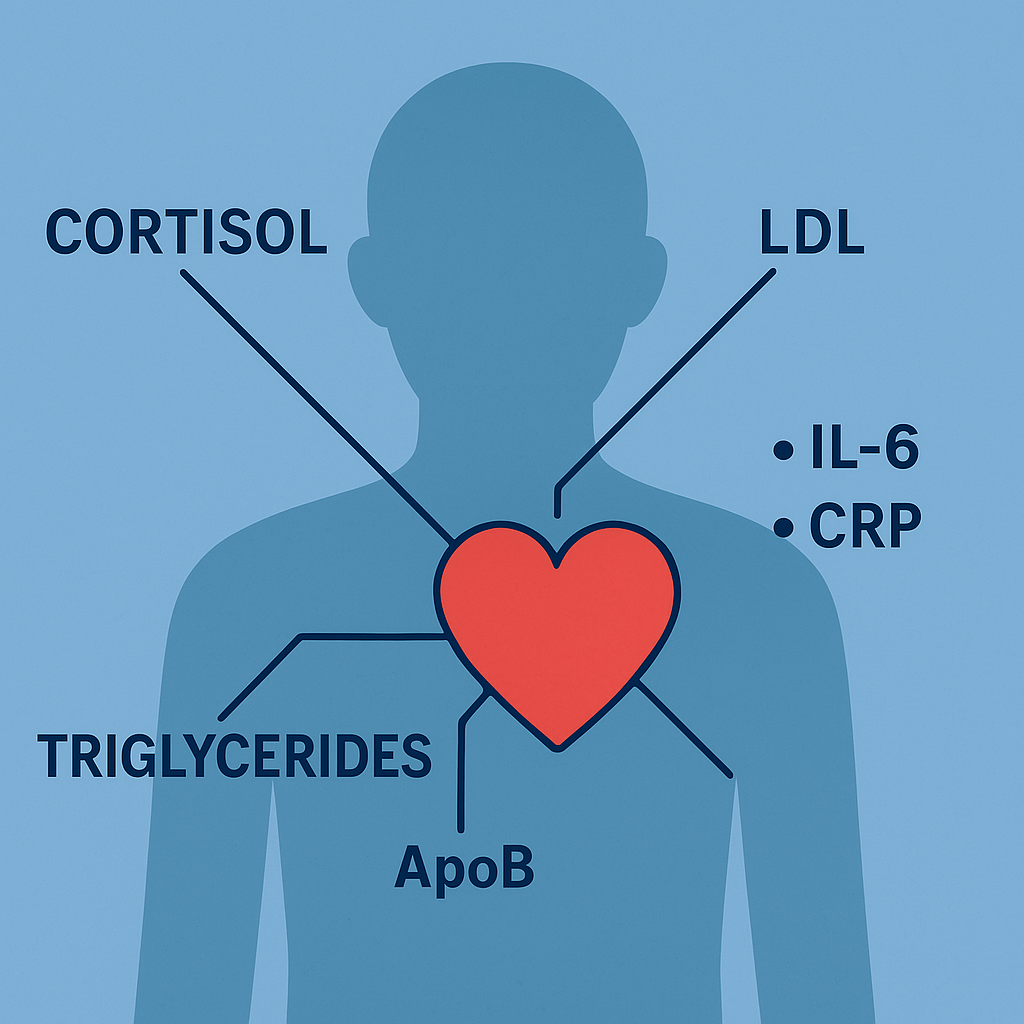
1. The Role of Stress and Cortisol in Heart Health
We often think of heart disease in terms of diet or genetics, but one of the more silent and underestimated risk factors is chronic stress.
When you’re stressed—especially for prolonged periods—your body releases a hormone called cortisol. In small, short-term doses, cortisol is helpful. It gives us energy and focus in times of need. But when cortisol remains elevated day after day, it starts to take a toll on the body.
High cortisol levels have been linked to:

-
Increased blood pressure
-
Elevated blood sugar
-
Weight gain, particularly around the abdomen
-
Suppressed immune function
-
Higher LDL (bad) cholesterol and triglyceride levels
Over time, this chronic stress response contributes significantly to heart disease. One of the best preventative measures you can take is to actively manage your stress. This doesn’t mean eliminating all sources of pressure from your life (which isn’t realistic), but rather incorporating stress-reducing habits like mindfulness, regular exercise, restorative sleep, and perhaps supplementation that supports a healthy cortisol response.
2. Understanding and Managing LDL, Triglycerides, and ApoB
When we talk about cholesterol, most people think in terms of “good” (HDL) and “bad” (LDL) cholesterol. But the picture is a bit more complex.
LDL (Low-Density Lipoprotein):
This is traditionally labeled the “bad” cholesterol because high levels can lead to plaque buildup in your arteries. However, not all LDL is created equal. What matters more is the number of particles and their size. Smaller, denser LDL particles are more likely to penetrate the arterial wall and contribute to atherosclerosis (plaque buildup).
Triglycerides:
Triglycerides are a type of fat in your blood. After you eat, your body converts calories it doesn’t need into triglycerides, which are then stored in fat cells. High levels of triglycerides are associated with an increased risk of heart disease and often occur in people with insulin resistance or poorly managed diets high in sugar and processed carbs.
ApoB (Apolipoprotein B):
If you really want to get a clearer picture of your cardiovascular risk, look at your ApoB levels. ApoB is a protein found in all atherogenic (plaque-causing) particles, including LDL and very-low-density lipoprotein (VLDL). Measuring ApoB gives you a more precise count of the number of potentially harmful particles in your bloodstream—regardless of how much cholesterol they carry.
In short: LDL and triglyceride levels are important, but ApoB is emerging as a better predictor of risk because it tells us how many dangerous particles are floating through your arteries.
Preventative takeaway: Keep an eye on your lipid panel, but also ask your doctor about getting your ApoB measured. Targeting lifestyle changes or supplements that help reduce LDL, triglycerides, and ApoB particle count can dramatically reduce your heart disease risk before any symptoms appear.
3. The Hidden Risk: Chronic Inflammation
Cholesterol isn’t the whole story. You can have perfectly “normal” lipid levels and still be at risk if your body is in a state of chronic inflammation.
Two key inflammatory markers to know about are:
-
IL-6 (Interleukin-6): A cytokine that plays a role in immune response. Elevated IL-6 levels are associated with chronic inflammation and have been linked to atherosclerosis and plaque instability.
-
CRP (C-reactive protein): Produced by the liver, CRP levels rise when there is inflammation in the body. High-sensitivity CRP (hs-CRP) is particularly useful in detecting low-grade inflammation that contributes to heart disease.
Inflammation damages the endothelium (the inner lining of the blood vessels), making it easier for cholesterol particles to stick and form plaques. It also destabilizes existing plaques, increasing the risk of sudden rupture and clot formation—a major cause of heart attacks.
Even if your cholesterol is under control, inflammation can still be silently putting your heart at risk.
Preventative takeaway: Reducing inflammation is key to a comprehensive heart health strategy. That means prioritizing an anti-inflammatory diet rich in omega-3 fatty acids, colorful vegetables, and low in refined sugars and processed foods. Regular physical activity, sleep, and stress reduction also help. Certain supplements can further help target inflammatory markers like IL-6 and CRP.
4. Prevention vs. Reaction: Why Waiting for a Diagnosis is Too Late
Most people don’t take heart health seriously until they’ve had a scare—a high blood pressure reading, a borderline cholesterol result, or worse, a cardiac event.
But by the time these warning signs show up, much of the damage may already be underway.
The truth is, heart disease builds silently over years, often decades. Arterial plaques don’t form overnight. Chronic inflammation doesn’t pop up in a week. These are slow processes that respond best to slow, consistent action—the kind that comes from prevention, not reaction.
When we focus only on treating symptoms after they arise, we miss out on the opportunity to build true, long-lasting resilience. Prevention is the only strategy that keeps the foundation strong.
5. Building Your Preventative Plan
So how can you put all this into practice? Here’s a simple framework to guide your heart health plan:
Daily Habits:
-
30 minutes of moderate activity (like walking, cycling, or swimming)
-
At least 7 hours of quality sleep
-
Stress-reducing practices (like meditation, journaling, deep breathing, or even taking a walk outside)
Nutrition:
-
Focus on whole, minimally processed foods
-
Include healthy fats (like avocado, olive oil, nuts, and fatty fish)
-
Cut back on sugar and refined carbs
-
Stay hydrated
Labs to Monitor Annually:
-
LDL, HDL, and Triglycerides
-
ApoB levels
-
hs-CRP
-
Fasting insulin and glucose
-
Cortisol (if stress is a concern)
Supplements and Support:
Adding targeted supplements to your daily routine can complement your lifestyle changes, especially when it comes to reducing LDL, ApoB, triglycerides, and inflammation, or supporting a healthier stress response.
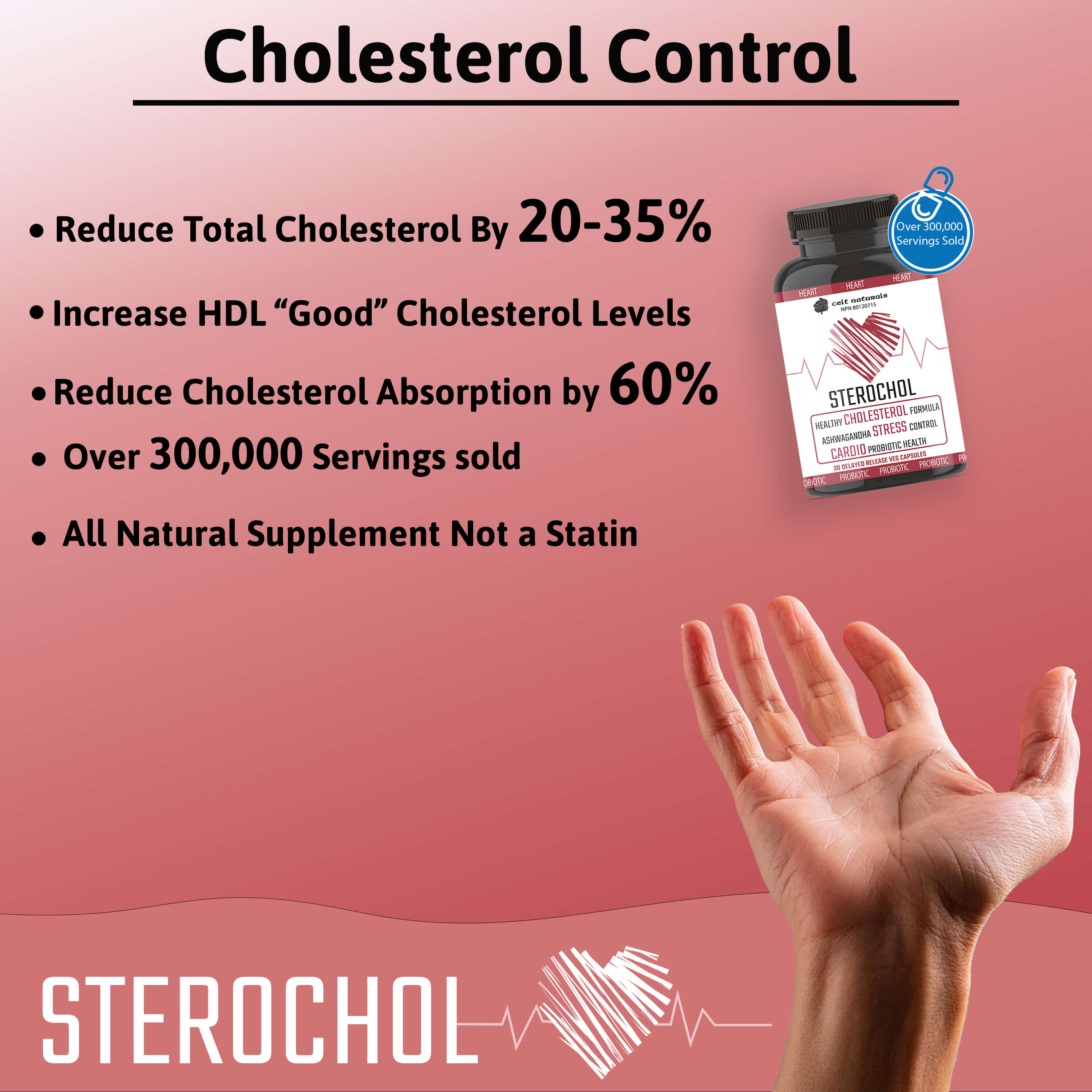
6. A Smarter Way to Support Your Heart
Taking care of your heart is not just about reacting to bad news—it’s about building a strong defense now. At Celt Naturals, we believe in a proactive, natural-first approach to health. That’s why we created Sterochol, a supplement specifically formulated to support a healthy lipid profile, lower inflammation, and reduce cortisol—all using clinically studied natural ingredients like plant sterols, ashwagandha, and Lactobacillus plantarum.
While no supplement is a silver bullet, Sterochol is designed to work in tandem with your healthy lifestyle to help keep your heart in its best shape—for the long haul.
Ready to take a proactive step toward better heart health? Make prevention a priority—not just a reaction. Your future heart will thank you.